What is the 6 Minute Walk Test Distance?
The 6-minute walk test (6 MWT) is easy to carry out and a practical test that is used to evaluate patients suffering from a variety of cardiopulmonary diseases including PAH. It only measures the distance a patient can take in 6 minutes to walk on a flat hard surface. However, the results reflect the integrated physiological response of complex physiology involving pulmonary and cardiovascular systems and neuromuscular circulation.
A level that reflects maximal consumption of oxygen stabilizes the metabolic rate; thus the test is a good measure of the capacity of aerobic exercise.
In patients with significant PAH, the correlation with the maximum cardiac output makes the test an indirect measure of the right ventricular function. The clinician who uses this test to evaluate PAH patients’ needs to be able to understand the 6MWT indications, logistics, limitations, and interpretations.
History of 6MWT
The 6MWT has been used in a number of medical conditions affecting the cardiopulmonary system as a relatively simple measure of aerobic exercise capacity. This six minute walk test is 'unencouraged' and thus 'self-paced' at a lower exercise level. The patients decide their own effort intensity, which more accurately reflects each individual's "everyday activities." The 6 minute walk test norms should be recognized as a global evaluation and does not specify the source of the limitation.
How to use 6MWT Calculator?
- select patient gender
- Enter Patient height and weight after selecting known units
- Patient age in years
- Enter Total distance covered by the patent
- Click on the "Calculate" button
you will get the answer in the result section. The 6MWT Calculator result will show you the predicted distance in meters and percent.
Technical Aspects
While guidelines are straightforward for the patient and administrator of the test, several technical aspects of the 6MWT require attention. The patient is advised to put his or her regular walking aids (e.g., walkers, canes) and comfortably dress in the appropriate footwear. We recommend a light pre-test meal. Two hours before the testing, exercise should not be done by the patient.
The patient must also rest 10 minutes before the walking test, after which vital signs including oxygen saturation are evaluated. The test is carried out at an unencouraged intensity, as previously mentioned. Furthermore, during the test, the patient can stop and rest. The patient should assess the level of dyspnea in a validated scoring system like the Borg dyspnea value, both at the basis and at the end of the test.
It is important not to ask for the "practice" walk from the patient. In fact, the patient should rest for an hour and the longest distance recorded if the walk test has to be repeated for a clinical purpose. A pulse oximeter, a timer, and blood pressure cuff are included in the necessary equipment.
Efforts should be made to create conditions which create an environment that reflects the normal functional status of the patient. For example, the patient should be provided with appropriate support for transporting oxygen if he or she uses activity oxygen. If the patient depends on oxygen, an adequate provision should be made. The test technician must not push the oxygen supply unit for the patient.
Some individuals may need to push or pull a mobile chair while walking. Luckily, advanced training facilities are not necessary. For measuring the distance in feet or meters, a lobby marked with a lap counter and/or pedometer may be used. An automatic defibrillator (AED) is also reasonably available.
Clinical Indications and Contraindications
Indications for the 6MWT
| Treatment Comparison | Functional Status | Outcome Assessment |
|---|---|---|
| Pulmonary hypertension | Pulmonary hypertension | Pulmonary hypertension |
| COPD | COPD | COPD |
| Heart failure | Heart failure | Heart failure |
| Pulmonary hypertension | Cystic fibrosis | |
| Lung resection | Peripheral vascular disease | |
| Lung transplant | Fibromyalgia | |
| Lung volume reduction surgery | Older patient |
Indications for the 6MWT
| Absolute | Relative |
|---|---|
| Unstable angina | Resting tachycardia (120) |
| Recent myocardial infarction | Poorly controlled systemic hypertension (MAP ≥135) |
| Unable to ambulate |
Patient Characteristics Or Conditions That Influence The 6-Minute Walk Distance Independent Of Cardiopulmonary Status
| Shorter Distances | Longer Distances |
|---|---|
| Short stature | Tall statures |
| Older age | Younger age |
| Women | Men |
| Comorbidities | Prior 6MWT |
Variability
Some factors determine variability between age, sex, anthropometrics, and comorbidities for a 6-minute walk distance between patients (cognition impairment, cardiopulmonary disorder, anemia, musculoskeletal limitations). In a single patient (e.g. serial testing), variability may also be seen. Before testing, the distance patient walked ("learning effect ") should be increased. Ideally, comparative tests should be carried out during the day at similar times.
It is possible to reproduce both "encouraged" and "unencouraged," but to remove variability, the process needs to be standardized. The phrase "go as quickly as you can, "in order to avoid premature fatigue or other symptoms, may be best avoided. If possible, use the same flow rate. If a flow rate increase is required in the clinical situation, this should be adequately documented.
Additional technical problems should be noted that can introduce variability. The interaction between the patient and the person who performs the test may lead to the patient 'tracking' the pace of the tester. The technician must not go with or before the patient in order to avoid such a confusing factor. If the technician needs to accompany the patient to monitor data or to ensure patient safety, the technician is advised to walk behind the patient in order to settle the pace of walking.
The interface (nasal cannula, oxygen transtrache or oxygen mask) and the delivery of flow (continuous or pressed) must be noticed for variation in oxygen supplies (portable concentrate, fluid or gas tank). If an adjustment to the oxygen flow is needed during the walk test, the reason should be documented.
The test results may also be affected by medications (type, dose and administrative time) and should also be documented carefully. For the prediction of normal6-minute journey distance based on several variables, reference (normative) equations are available.
Even with this kind of equations, 60% of the difference remains within 6 minutes-walk. Furthermore, while the percentage predicted value can contribute to the analysis of the 6mwt norms, its predictive value does not exceed the absolute distance. In subjects older than 40 years, normative equations were developed to ensure caution in the application for patients younger than that.
Interpretation
The 6-minute distance change can be applied to assess the effectiveness of a workout or, over time, to track the natural history of changing the exercise capacity. The 6MWT is most frequently used as a base and follow up evaluation after a particular procedure or in monitoring the progression of the disease. Unfortunately, this comparison was not ideally represented.
The options available include: absolute distance difference as compared to a normal, change in the percentage. The clinical difference of minimal importance for lung vascular disease has not been determined. Both chronic obstructive and interstitial lung diseases are subject to criteria.
In tradition, the minimum significant difference (i.e., improvement) in the distance walks of 6 minutes (with a confidence limit of 95% to 37 to 71 meters) has been estimated to be 54 meters. For chronic obstructive or interstitial pulmonary disease patients, the value may be lower. For comparison to the previous testing, the percentage change of distance traveled may also be used.
Prognosis
The early literature used a breakpoint 332 meters to demonstrate a relationship to the three- year survival. The distance was less than 332 meters compared with 92% if it was higher, only 20% of patients lived 3 years. The 6MWT was evaluated on evidence-based clinical guidelines in the American College of Chest Physicians. The quality of evidence used for exercise tolerance in the monitoring of patients with a net "substantial "benefit was determined as "good. "
Overall, the strength of the PAH recommendation was an "A. "In an objective approach to the treatment of PAH, a longer distance of 380 meters had been used. The correlation with results and emphasis on objective therapy goals has led to recommendations on the risk stratification of the distance. Such advice is based on the poor result of a short distance and involves the use of more "aggressive "therapies such as infusion prostacyclin. Such a treatment selection approach has perhaps not been proven to be reasonable.
Specific Issues of 6-MINUTE WALK TESTING in PAH
The 6MWT is commonly employed in diagnosis and evaluation of PAH patients. The 6MWT diagnosis is commonly used in PAH patients. In the cardinal studies of idiopathic PAH intravenous epoprostenol, the test calculates aerobic exercise capacity and corresponds to cardiac output, thereby making the results and the indirect measurement of right ventricular function possible.
In most of the efficacy studies of the current FDA-approved pulmonary arterial vasodilator therapy since then, treatment-related improvements for PAH patients over the 6-minute walk distance have been used as primary endpieces. The test has not been standardized in PAH patients despite its extensive deployment in the pulmonary vasodilator trials.
We feel that 6 minute walk test vary between institutions from conversations with personnel at other pulmonary hypertension (PH) centers. Although most centers strive to comply with the recommendations of the American Thoracic Society, certain differences are dictated by the architectural design of the test facilities. One example is the use of a single hallway versus a continuous path. In many of the pulmonary vasodilator studies, recommendations for the performance of the 6MWT were provided in the protocol; however, the level of specificity and consistency in the test varied.
There are significant differences in six minute walk test understanding and interpretation for patients with pulmonary vascular disease in the absence of broad standardization. The combination of simplicity of the examination and its consistent application in efficacy studies nevertheless led to widespread use in patient clinical evaluations. The currently available clinically based guidelines have recommended serial measurements. The 6MWT can be used to assess the progression of both disease and clinical therapy reaction.
6 minute Walk test norms
References
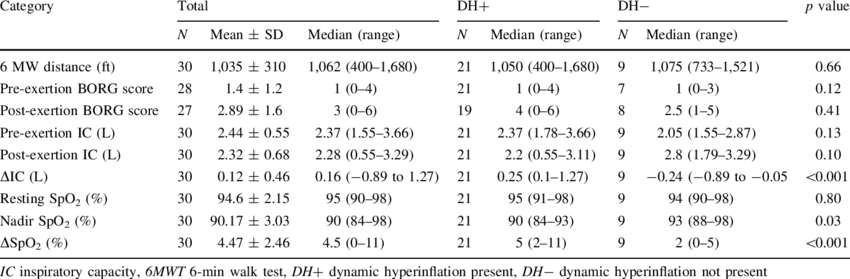
Zafar, Muhammad & Tsuang, Wayne & Lach, Laura & Eschenbacher, William & Panos, Ralph. (2013). Dynamic Hyperinflation Correlates with Exertional Oxygen Desaturation in Patients with Chronic Obstructive Pulmonary Disease. Lung. 191. 10.1007/s00408-012-9443-3.